What’s striped, native to Southeast Asia and regrows spinal neurons in under 10 weeks?
Zebrafish, or Danio rerio, could just be the key to unlocking regeneration in humans. On Sept. 18, Valentina Cigliola, an assistant professor from Vanderbilt University’s Department of Pharmacology, presented her talk titled “Innate Mechanisms of Spinal Cord Regeneration,” hosted by Assistant Professor of Biology at Hopkins Erin Jimenez. Her talk centered on how understanding the innate mechanisms of spinal cord regeneration in zebrafish may reveal to us how to induce regeneration in adult mammals.
It comes as no surprise that humans don’t possess the same magical healing as our zebrafish counterparts. Various types of human tissue are unable to regenerate after injury, such as the brain, heart and spinal cord, but Cigliola focused on the particular dangers of spinal cord lesions.
“Spinal cord lesions affect up to 500,000 people every year worldwide and lead to irreversible paralysis because no known method exists to restore the tissue once it scars,” Cigliola noted.
In order to develop treatments and cures for serious spinal injuries, scientists have turned to model organisms that survive and thrive after spinal injuries. Researchers have decided to focus on zebrafish, not for their flashy stripes, but for their remarkable regenerative abilities. After spinal transections (where a cut is performed on the spine of the zebrafish), zebrafish can form a “tissue bridge” composed of glial cells (which are dedicated to neural homeostasis) woven around the injury site. These bridges reconnect the two severed areas, allowing axons to regrow and eventually restoring swimming ability to the fish. This entire process is a far cry from the fibrotic scarring that walls off injuries in mammals, which prevents any type of true neural regeneration.
Cigliola’s lab was curious about the cells involved in the tissue bridge. Why was it that progenitor neural cells were responding and dividing in zebrafish neural injuries, but not in humans?
“What drives neurogenesis from ependymo-radial glial (ERG) progenitors? That was the question we were working hard to understand,” Cigliola explained.
The answer? Cigliola’s lab zeroed in on heparin-binding epidermal growth factor a (hb-egfa), a factor that is high in ERG progenitors following injury. Using transgenic zebrafish, this factor, when unregulated in cells, kicks off neurogenesis and axon extension. The opposite also held; when hb-egfa was genetically knocked out, zebrafish had dramatically reduced tissue bridging, weaker axon growth and poorer swim recovery, compared to their wild type counterparts. These findings emphasize how hb-egfa is deeply important for regeneration and effective recovery from spinal injuries.
Interestingly, administering human-derived hb-egfa protein to zebrafish rescued many of these deficits, hinting that the human version of hb-egfa is also capable of tissue regeneration in mammals. However, dosing adult mammalian spinal cord with zebrafish-derived hb-egfa provided little to no injury response, opening up a whole new box of questions. Was hb-egfa the only signaling mechanism for tissue bridging and regenerative work, or was something else involved?
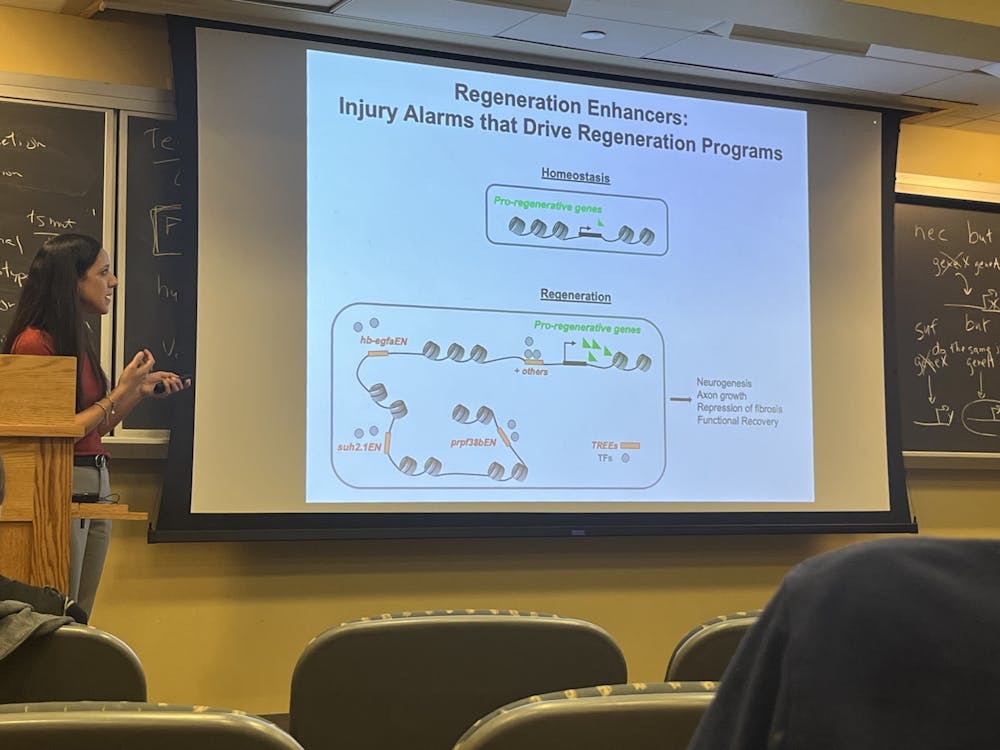
Turns out, hb-egfa was not the only factor involved in mammalian neural regeneration, and the other component of neural regeneration may lie in the trees. Well, not the type of tree you’re probably thinking of. Cigliola highlighted a set of DNA sequences her team calls “TREEs,” Tissue Regeneration Enhancer Elements, which act like injury alarms embedded in the genome. These TREE sequences switch on regeneration-focused signaling pathways focused only at the injury site and then shut off after repair is complete.
Yet, most of these enhancers aren’t conserved in mammalian genomes, which may explain our limited regenerative capacity, but mammalian transcriptional machinery can still “read” the fish enhancers when they’re engineered into mice, suggesting that some of the TREEs-associated signaling pathways are still intact in mammals.
Now, the team’s most recent experiments focus on adeno-associated viruses (AAVs) to deliver zebrafish enhancers linked to human hb-egfa into neonatal mouse spinal cords. Cigliola reported findings of increased axon density after injury, an encouraging first step toward “teaching” mammalian tissue to behave more like their fishy counterparts.
If the ultimate goal is to induce regeneration in adult humans, these results point to a promising strategy against crippling injuries: provide the right growth factors (like hb-egfa) and the right genetic “switches” (like TREEs) to turn them on only where and when needed, like severe injuries.
For now, zebrafish remain the magical wizards of spinal cord repair. But as Cigliola’s research revealed, their genetic toolkit may one day let us write a happier ending for human injuries too.
Cigliola’s presented research: https://pubmed.ncbi.nlm.nih.gov/32461216/
Editor’s Note, 2025: An earlier edition of this article inaccurately stated that the tissue bridge was also composed of fibroblasts, in addition to glial cells. The News-Letter regrets this error.