Artificial intelligence-based protein structure prediction and protein design tools have revolutionized structural biology. Chief among these tools is AlphaFold, which was developed by researchers at Google DeepMind and recently won the 2024 Nobel Prize in Chemistry. AlphaFold was trained on existing protein structures, which makes it extremely proficient at predicting the structure of stable proteins with well-characterized domains. However, it struggles with predicting the structures of misfolded proteins and intrinsically disordered domains, which are prevalent in many degenerative diseases such as Alzheimer's Disease, Parkinson's Disease, Huntington's Disease, Amyotrophic Lateral Sclerosis and cystic fibrosis. Therefore, it is crucial to study how proteins related in these diseases misfold in order to understand the pathologies and develop treatments and cures for these diseases.
Stephen Fried is an associate professor in the Department of Chemistry at Hopkins who is working on this exact problem. After attending the Massachusetts Institute of Technology for his undergraduate studies, he joined the Steven Boxer lab in the Department of Chemistry at Stanford. In an interview with The News-Letter, Fried emphasized the importance of his PhD training and mentorship in influencing his scientific journey and bringing him to his current post at Hopkins.
“[Boxer] could make anyone in the room passionate about [his work],” he said. “He has that charisma — that way of explaining things that made them sound interesting, even if you had never thought about it two minutes ago.”
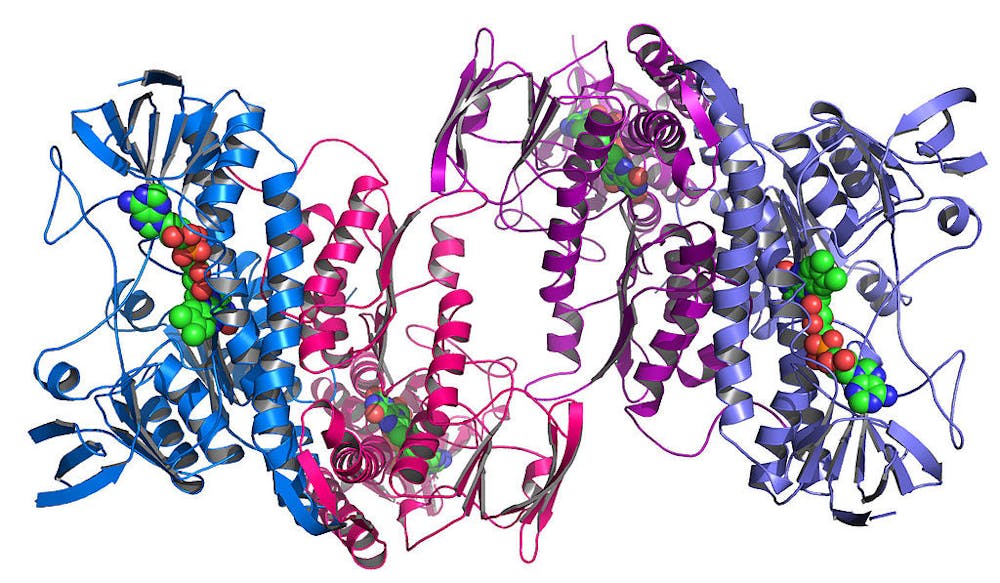
For his doctoral thesis, Fried worked on a bacterial enzyme known as ketosteroid isomerase (KSI), which intrigued him because it possessed the highest rate constant of any known enzyme at the time. He found that the electrostatic environment in KSI was perfectly tuned to stabilize the charge rearrangement needed to access the rate-limiting step of the reaction.
“A PhD is a really unique time in your life when you can focus on one project and have a lot of agency and control over how that evolves, and be responsible for the creation of new knowledge,” Fried said.
As a principal investigator, Fried has continued to study proteins and now specializes in protein folding and misfolding.
“In biophysics, there is a common belief, [known as the Anfinsen dogma,] that all of the information that a protein needs in order to fold into the right 3D shape that we call the native structure is somehow present in the amino acid sequence,” Fried said. “One way that you can critically test this theory is you can basically take a protein that came from a cell that has the right string of amino acids attached to each other, and, using a chemical, basically cause the protein to come apart. We call those denaturants.”
When Fried’s group performed the denaturation experiment with many different proteins, they saw that Anfinsen’s dogma held for small, simple proteins. However, as proteins became more complex, they were unable to refold properly. So in order for these complex proteins to fold into their native states, the cell had to contain separate machinery to assist folding.
This observation brought Fried to consider protein misfolding in neurodegenerative disorders.
“It’s long been thought that there is a contribution from protein misfolding in neurodegenerative disease. If you look inside the brain tissue of a person who had a very severe case of these diseases, what you find is that there’s a lot of degeneration and, where there used to be and where there should have been neurons, instead you see these ugly deposits of misfolded, aggregated proteins,” Fried said. “In Alzheimer's disease, we see a lot of a protein called amyloid beta and tau. And in Parkinson's disease, we see alpha synuclein.”
Currently, in the field of neurodegenerative disease research, scientists are split over the idea that these aggregates directly cause disease. For example, many therapies have been developed to reduce amyloid beta aggregates in patients, but these clinical trials have had indeterminable effects on cognitive function.
“As we start to look closer at how proteins are looking inside the brain, [...] we are finding that there are a lot of proteins that are not in their native shape,” Fried said. “We just haven’t known this because it takes more sophisticated methods to detect these more subtly typse of misfolding — they misfold without forming amyloids.”
To test the presence of additional misfolded proteins, Fried’s group used a technique known as limited proteolysis mass spectrometry. This method involves extracting proteins out of both neurotypical brain tissue and diseased brain tissue, followed by protease digestion — which cuts protein domains that are more flexible or more exposed — and subsequent mass spectrometry. If a protein is properly folded, performing mass spectrometry should result in identical fragments between the neurotypical and diseased brain. However, Fried’s group found many mass spectrometry profiles that differed between the two samples in addition to amyloid-forming proteins, meaning that there were more misfolded proteins involved in neurodegenerative diseases than previously believed.
Though Fried has not determined a specific mechanism for protein misfolding in neurodegeneration, he believes that it has to do with the increased stability of improperly folded proteins.
“There are ways that proteins can misfold that [...] impairs their function, [and] also their turnover. So instead of having a lifetime of two weeks, the misfolded protein now has a lifetime of a month,” Fried said. “So over time, you're slowly accumulating this misfolded protein, [...] because it’s not getting broken down as quickly as it should be.”
Fried believes that it will ultimately take much more dedicated study to find the root cause of neurodegenerative conditions like Alzheimer’s and Parkinson’s.
“When it comes to these diseases, we still have a lot more basic stuff to learn, because we're still arguing about what causes the disease in the first place,” he said. “What we're looking at when it comes to neurodegenerative disease is still [murky].”