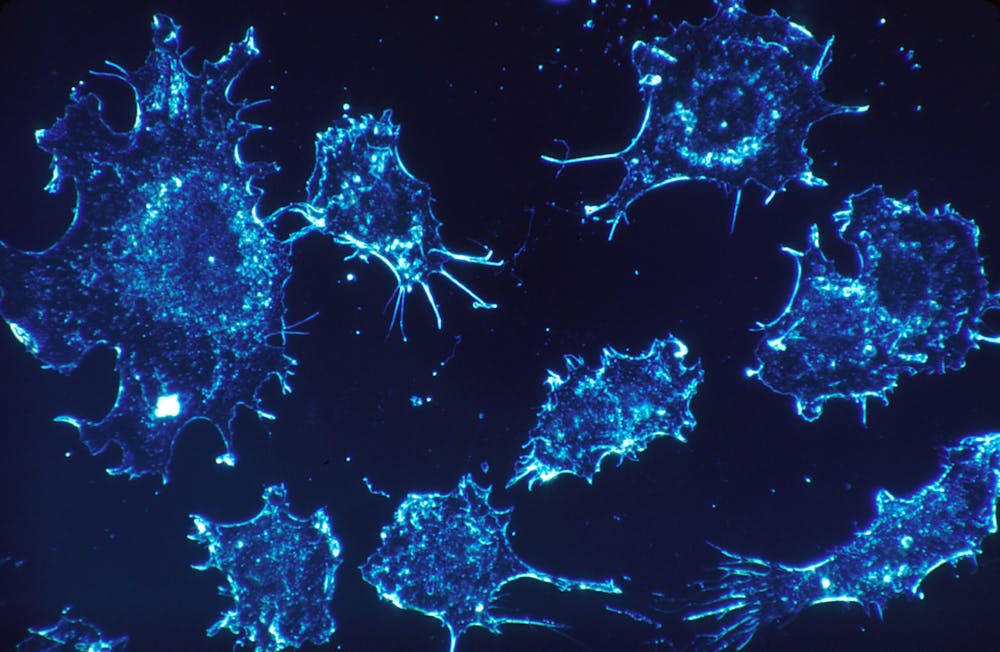
On Tuesday, Nov. 7, Peng Jiang, a Stadtman investigator for the Cancer Data Science Laboratory, held a talk discussing the role of big data approaches in studying intercellular signaling — specifically, how cancers evade immune system function in humans. The talk was titled “Big Data Approaches to Study Intercellular Signaling During Tumor Immune Evasion” and was hosted by the Institute for Computational Medicine and the Department of Biomedical Engineering at Hopkins.
Big data refers to, quite literally, large datasets. It is often multidimensional and can be computationally analyzed to reveal trends in a particular dependent variable. The advancement of modern biomedical research and clinical care has generated rich datasets that can be analyzed using artificial intelligence (AI) approaches.
Cancer research in particular benefits from the use of bioinformatics and AI. By applying novel computational methods to datasets such as The Cancer Genome Atlas and The National Center for Biotechnology Information Gene Expression Omnibus database, researchers can gain a deeper understanding of cancer progression and develop novel insights into cancer diagnosis and treatment.
Jiang shared three computational frameworks, developed by his team, to study intercellular signaling and cell-cell communication in the antitumor immune response.
The first model was the Cytokine Signaling platform (CytoSig) which aids in studying the cellular response to signaling molecules, specifically focusing on cytokines secreted by immune cells. Cytokines mediate interactions between cells to promote tumor growth.
Jiang emphasized the difficulties the researchers faced in data collection for CytoSig.
“The first step of building up a computational framework is always data collection,“ Jiang explained during the talk. “The key challenge is that the metadata… is very heterogeneous. For example, what cell lines [are involved], what treatment conditions… it’s very hard to uniformly… homogenize the metadata to do algorithmic analysis.”
Jiang further explained how CytoSig provided new insights into the cross-regulatory cascade of cytokines, or how cytokines upregulate and downregulate one another. The model also revealed previously unidentified roles of many cytokines. For example, it identified cytokine BMP6 as an anti-inflammatory factor and found new candidate therapeutic targets to treat human inflammatory diseases, such as targeting CXCL8 for severe COVID-19.
Jiang then moved on to discuss the tumor-resilient T cell (Tres) model. T cells are white blood cells that either release signaling molecules or directly kill foreign cells to aid in the body’s immune system. Tres uses RNA-transcript data to identify T cells in the immune system that are resilient to immunosuppressive environments, or environments similar to tumor cell environments where immune system function is suppressed. The model was developed in response to the low efficacy of immunotherapy in solid tumors.
Jiang highlighted two main stages of the development of Tres. In Stage 1, the researchers used CytoSig to quantify immunosuppressive cell signaling. Next, Tres was used to look at which T cells are resilient in immunosuppressive states in solid tumor masses.
Jiang discussed the vision behind the Tres research and the main goals the researchers hoped to achieve.
“Tres is looking for the molecular markers of T cells that are still proliferating even under immunosuppression. Using this model, we can compute a score for each gene,“ Jiang said at the event. “So the key question is: Could we get any human clinical outcome prediction using [Tres]?”
Jiang then outlined how researchers evaluated the Tres model using the Pearson correlation coefficient as an output. If the value was positive, the model predicted that immunotherapy would be effective. If it was negative, the model predicted that immunotherapy would be ineffective. The researchers found that Tres’ predictions were generally consistent with clinical outcomes. Tres also identified the FIBP gene as a marker of low T cells across many solid tumor types, hinting at a new potential target for immunotherapies in solid tumors.
In the final third of his talk, Jiang delved into the Spatial Cellular Estimator for Tumor (SpaCET) model, which uses spatial transcriptomics (ST) data. ST maps RNA transcripts to tissue samples and cell types to infer cell identities within tumors.
Spatial transcriptomics is a popular area of current research in computational medicine, but past models before SpaCET did not adequately address the challenges of analyzing tumor ST data.
“There are a few other similar computational frameworks published before [SpaCET]... Lots of true challenges about spatial transcriptomics are not really sufficiently addressed by previous approaches,” Jiang said.
Cells in tumors are arranged irregularly, resulting in asymmetry in cell density across the tumor. Current models get past this issue by calculating cell fractions and normalizing them to one value across the tumor, erasing the complexity due to irregularity in tumor densities.
Jiang explained that to address the challenge of tumor irregularity, the researchers used two main dimensions in their tumor ST data: copy number alterations (CNAs) and malignant transcriptome signatures. Researchers matched ST data from each tumor to datasets with expression profiles of malignant cells that had the same CNAs or the same transcriptome signatures. By accounting for heterogeneity within a tumor, SpaCET was able to study cell-cell interactions in multicellular ST data more effectively. This would eventually allow clinicians to better understand how the interaction between tumor cells and immune cells contributes to cancer progression.
Jiang concluded the talk by discussing the focus of his current work.
“Recently we are intensively focusing on how to use ST data and approaches to identify new secretory proteins [and] ligand-receptor interactions underlying cancer immunotherapy response and resistance,” Jiang said.
Jiang’s past and current work holds great promise in understanding the mechanism of tumor cells’ resistance to immunotherapy; his work develops computational models that can aid clinicians in understanding how cancer evades the immune system and predicting the efficacy of immunotherapy in cancer patients.