Macy Early, Dr. Lydia Pecker and other researchers at Hopkins recently found a higher risk for severe maternal mortality (SMM) among patients with sickle cell disease (SCD) than those without. The study also identified a racial disparity; Black SCD patients had a 10% higher SMM. Their results were published in Jama Network Open.
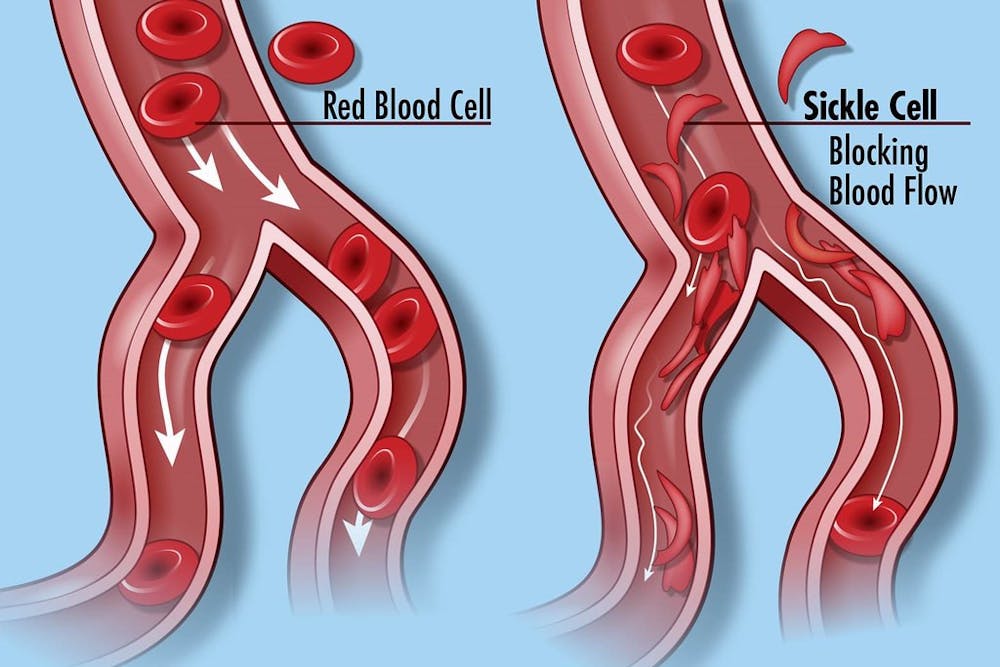
SCD is an inheritable disease through an autosomal recessive pattern, which means one would only be affected if they receive the gene from both parents. SCD patients have abnormally-shaped hemoglobin, a protein in red blood cells whose defect interferes with oxygen delivery throughout the body. Rather than the usual disk-like shape, red blood cells among SCD patients look like a crescent, or sickle, which can increase the risk for blockage of blood vessels due to difficulty of movement.
The mortality found in Early’s study was higher than the last reported statistics in an epidemiologic paper in 2008, though both sickle cell disease care and pregnancy care have improved since then. The study found a 26% elevated risk for SMM in pregnant patients with SCD.
Early, the lead author on the study, is a fourth-year medical student at Hopkins.
In an interview with The News-Letter, Early explained the motivation behind choosing to study pregnancy in relation to SCD. She noted that the body undergoes many physiological changes during pregnancy. The researchers wanted to investigate how these changes interact with SCD’s chronic traits.
Additionally, Early highlighted that women’s health is systematically understudied and receives less research funding from National Institutes of Health.
“The population of interest in this study, pregnant patients with SCD, includes both women and African Americans who are traditionally underserved populations. They are in very much need for study and investment,” she said.
SCD has a higher disease prevalence and burden on Black individuals; according to the Centers for Disease Control and Prevention (CDC), SCD occurs in one in every 365 Black births. Worse pregnancy outcomes for Black individuals are not only attributable to SCD but also to systemic racism, such as unequal access to healthcare.
Given the relatively low prevalence of SCD in the U.S. — affecting only 100,000 Americans — there are even less SCD patients who are also pregnant. Therefore, a multicenter approach or even a national cohort is necessary to draw efficient conclusions about any relationship between pregnancy and SCD.
The researchers chose the National Inpatient Sample because of its breadth of data from nearly all inpatient care providers in the country. Although the data has flaws, such as the lack of vital or lab data, it representatively documents the scope of pregnant patients with SCD in the country, from academic centers to community hospitals.
The researchers used the SMM Index created by the CDC as a standardized measurement to benchmark the current state of outcomes for pregnant patients with SCD.
Pecker is an assistant professor of medicine at the Johns Hopkins Division of Adult Hematology, and she takes care of young adults with sickle cell disease at the Johns Hopkins Sickle Cell Center for Adults. Her research focuses on the fertility and pregnancy of women with sickle cell disease.
In an interview with The News-Letter, Pecker explained that the placenta and fetus are understudied end-organs (organs affected by a given disease) of SCD. Given academia’s apathy toward the intersection of women’s health and SCD, many needs of pregnant patients with SCD are not sufficiently understood or addressed.
“More knowledge about disease pathophysiology and more access to multidisciplinary comprehensive care are important,” she said. “Building off the first paper, Early published a companion paper comparing pregnancy outcomes between anemia patients and SCD patients. The study found similar complications between pregnant patients with anemia and those with SCD, such as the abnormal development of the placenta and cardiovascular stress.”
This paper also identified risks that are elevated only in SCD disease, such as acute chest syndrome and blood clots, both of which are due to the blockage of blood vessels by sickle-shaped red blood cells. The paper suggests that anemia, a symptom of SCD, may influence SMM in pregnant patients with SCD.
Looking ahead, Early and her colleagues want to gather multicenter prospective clinical data to develop evidence-based guidelines for treating pregnant patients with SCD and improving their health outcomes. There is a movement in the SCD community to create more comprehensive care centers, where SCD patients can receive specialty and multidisciplinary care to address their diverse needs.
The National Alliance of Sickle Cell Centers is working to define care standards across the country and enhance access to care for pregnant patients with SCD. Other countries, such as the UK, already have developed care guidelines for this population, which is something the U.S. currently lacks.
Pecker stressed the importance of studying SCD from both clinical and public health perspectives.
“Sickle cell disease is one of the great public health and biomedical challenges of our time. It is important to conceptualize SCD as having profound interaction between both the public health and biomedical systems,” she said.