In recent years, the opioid crisis has become one of the United States’ most pressing public health issues. Countless news articles, heartbreaking photos and harrowing documentaries have been released to the public in order to raise awareness about this unsettling issue.
As a result, there is a large chance that you’ve at least heard the terms “opioid crisis” or “opioid epidemic.” For example, in a 2018 survey conducted by The Associated Press-NORC Center for Public Affairs Research showed that the number of Americans who see opioid addiction as a significant issue for their community had significantly increased from 2016. This trend has not changed since then.
However, it is far less likely for an individual to be aware of what is being done to address this issue. Too often, Americans are made aware of public health issues by the media but fail to take the time to learn about possible solutions to these issues.
In the era of click-bait and fake news, the media has become heavily concerned about reporting only the most interesting of topics, preferring to cover the “outbreak,” “epidemic,” or “crisis” without honing in on solutions being investigated by smaller organizations.
This imbalance of information distribution led me to pursue my own research into what is being done to manage current public health crises, starting with the opioid crisis. While there are many different propositions regarding how to address this issue, I’ve decided to focus on one rather controversial way of managing the opioid crisis: supervised injection sites.
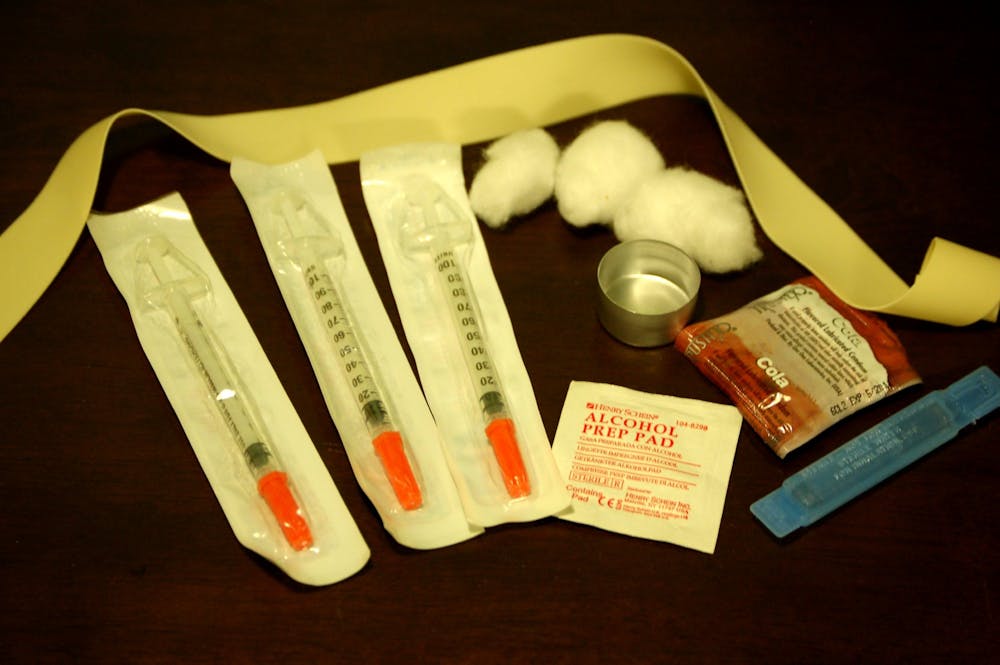
Supervised injection facilities, or SIFs, are specific sites where people who inject drugs (PWID) inject previously obtained drugs in the presence of trained medical professionals. Although the legality of these sites is often disputed, the need for them cannot be denied.
Overdose rates are on the rise in many U.S. cities due to a number of factors including an increase in prescription opioid abuse and the circulation of synthetic opioids like fentanyl, which is 50 to 100 times more potent than heroin and morphine.
In an effort to emphasize the amount of overdose deaths related to the abuse of opioids, I decided to focus on one city in particular: Baltimore. Baltimore has one of the highest overdose death rates in the country.
A 2018 report by Maryland’s Opioid Operational Command Center found that 800 of the 2,114 people that died from opioid overdoses died in Baltimore City. Six hundred thirty-nine deaths were reported in the first months of 2019. These numbers make it clear that SIFs, which reduce overdose deaths, are absolutely needed in cities like Baltimore.
Amos Irwin and colleagues published their cost-benefit analysis of a hypothetical supervised injection facility titled “Mitigating the heroin crisis in Baltimore, MD, USA” to the Harm Reduction Journal in 2017.
The study estimated the benefits by utilizing local health data and data on the impact of existing SIFs. Existing SIFs that have been studied include the Insite SIF in Vancouver, Canada and the Medically Supervised Injecting Centre (MSIC) in Sydney, Australia, which were established in 2003.
The study found that SIFs help prevent disease and infection. For example, SIFs reduce blood-borne disease transmission by providing clean needles and safer injecting education in addition to reducing bacterial infections by providing clean injection equipment.
Furthermore, the medical personnel at SIFs are responsible for many of the additional benefits provided by the sites. The staff reduces bacterial infections by cleaning wounds and identifying serious infections early, intervene in case of overdose and are able to persuade PWIDs to enter treatment after gaining their trust.
Finally, the study outlines the cost of a single SIF: “For the annual cost of $1.8 million, a single SIF would generate $7.8 million in savings, preventing 3.7 HIV infections 21 Hepatitis C infections, 374 days in the hospital for skin and soft-tissue infection, 5.9 overdose deaths, 108 overdose-related ambulance calls, 78 emergency room visits and 27 hospitalizations, while bringing 121 additional people into treatment.”
Overall, it is clear that SIFs are not only cost-effective, but also produce significant public health benefits — the most important being saving lives. Despite having such clear benefits, the eventual establishment of SIFs in the United States continues to be highly questionable.
This is due to both public and political concerns. Opponents argue that SIFs promote drug use and will bring PWIDs to neighborhoods where they are established. They also claim that SIFs are illegal under the federal Controlled Substances Act.
More specifically, two sections of the Controlled Substances Act could be interpreted to prohibit the establishment of a SIF: Section 844, which prohibits drug possession, and Section 858, which prohibits knowingly maintaining a place for the purpose of unlawfully using a controlled substance. President Trump and his administration have made it clear that they would pursue legal action against cities or states that allow SIFs.
Despite the aforementioned interpretations of the law, both states and local governments still have the ability to authorize SIFs. Explicit state authorization will clear the haziness surrounding the legality of SIFs statewide and has a strong chance of withstanding a challenge from the federal government.
A weaker option would be the authorization of SIFs at a local level. This was done with syringe exchange problems which operate in cities throughout the United States without state authorization.
With more and more research proving that addiction is a complex disease, I believe it is time to shift our perspective of drug abuse. The criminalization of addiction is not an adequate response to the growing prevalence of drug abuse in our society. It is clear that the opioid crisis is not an epidemic that can be swiftly put to an end.
According to the Centers for Disease Control and Prevention, an average of 130 Americans die every day from opioid overdose. If supervised injection sites were implemented in the United States, some of these lives could be saved. There is no reason for lives to be lost as our government and health system work to prevent further opioid abuse nationwide.