It has been proven that humans can survive without appendices, gallbladder, spleen and even parts of their pancreas and liver, but the lung has always been considered an essential organ. That is, until thoracic surgeons at Toronto General Hospital of University Health Network, successfully resected the infected lungs of a dying woman.
The surgeons were able to keep the woman alive for six days, allowing her to recover from the infection and receive a transplant.
The 32-year-old woman, Melissa Benoit, had been fighting cystic fibrosis for three years. She had been infected with the influenza virus, and the illness had left Benoit with inflamed lungs filled with blood, pus and mucous. Furthermore, her coughing fits were so severe that she had fractured her ribs. This limited the amount of air entering her lungs, and by the time she arrived at the intensive care unit in early April of 2016, Benoit was using a ventilator to help her breathe.
Once Benoit’s oxygen levels dipped below normal survival limits, the ventilation system could no longer supply her with enough air to survive any longer.
“The influenza tipped her over the edge into respiratory failure. She got into a spiral from which her lungs were not going to recover. Her only hope of recovery was a lung transplant,” Dr. Niall Ferguson, Head of Critical Care Medicine at the University Health Network (UHN) and Mount Sinai, said.
Benoit was first put on Extra-Corporeal Lung Support, which is a life-support technology, but Benoit’s condition only worsened, with the bacteria spreading from her lungs to the rest of her body and her organs beginning to shut down as she progressed into septic shock.
The only option at that point was a lung transplant, but the bacterial infection had made Benoit unable to receive a transplant until she fully recovered.
“This was bold and very challenging, but Melissa was dying before our eyes,” Dr. Shaf Keshavjee, Surgeon-in-Chief of Sprott Department of Surgery at UHN, said. “We had to make a decision because Melissa was going to die that night. Melissa gave us the courage to go ahead.” Dr. Keshavjee was one of the three surgeons who performed the lung-removal operation on Melissa.
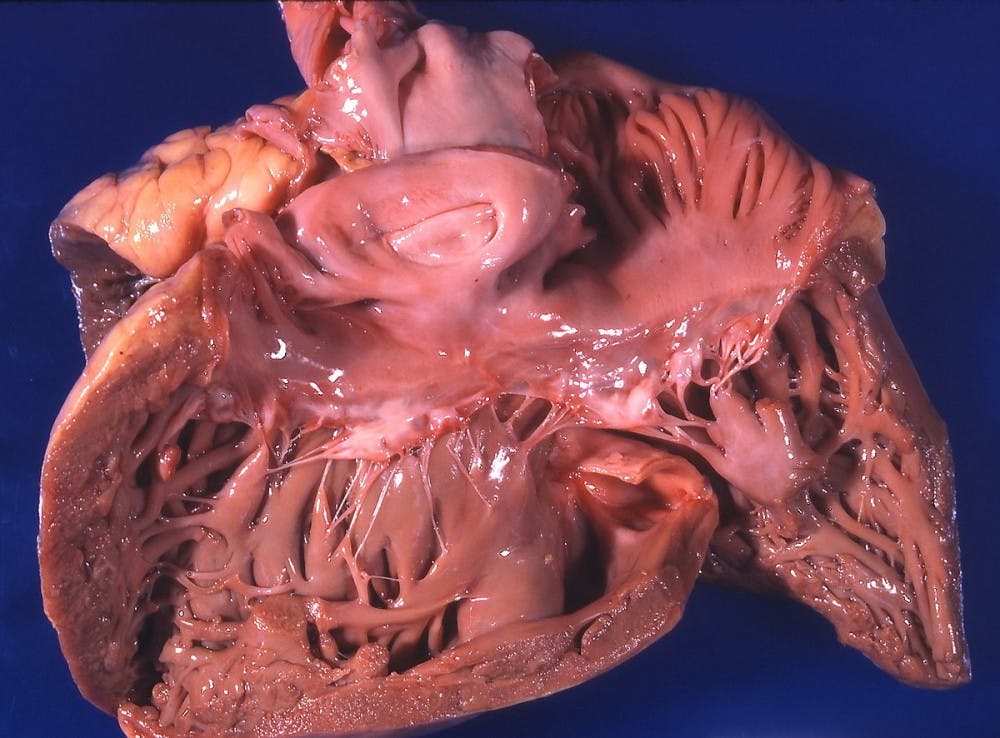
The surgical team decided to try a procedure that had never before been done. They planned to remove Benoit’s lungs to take away the source of infection, let her recover, and then insert the new lungs when she was ready. Although the procedure had many risks, including increased bleeding into an empty chest cavity and reduced blood pressure and oxygen levels to all-time lows, Benoit and her family were eager to go ahead with the plan.
“Things were so bad for so long, we needed something to go right,” Benoit’s husband Chris said in a news release, “and this new procedure was the first piece of good news in a long time. We needed this chance.”
The surgical team included three thoracic surgeons who worked to remove both of Benoit’s lungs during a nine-hour procedure. Benoit was then placed on advanced life support system, which included two external life-support circuits connected to her heart through tubes placed through her chest. An artificial lung known as the Novalung was used to add oxygen to her blood and remove carbon dioxide.
Within hours Benoit’s condition improved, and she was weaned off the medications as her organs began to function themselves. When she was ready six days later, Benoit received a lung transplant.
“The transplant procedure was not complicated because half of it was done already,” noted Dr. Cypel said. “Her new lungs functioned beautifully and inflated easily. Perfect.”
Benoit’s lung transplant was the first successful surgery of its kind. Benoit’s health condition has been only improving since her surgery.
Furthermore, the report of the surgery is published online in the November 2016 edition of The Journal of Thoracic Cardiovascular Surgery as “Bilateral pneumonectomy to treat uncontrolled sepsis in a patient awaiting lung transplantation.”