A big challenge in dealing with traumatic injuries to the brain is the limited regenerative capacity that the central nervous system has. Unlike skin or muscle, the brain’s ability to completely regenerate following injury is limited, often rendering the loss of brain function permanent following traumatic injuries to the brain or spinal cord.
However, recent research in neural stem cells offers much hope for future regenerative medicine to promote better functional recovery in individuals who suffered traumatic brain injuries. Studies suggest that the brain may be much better at self-repair than we previously expected, and augmenting the brain’s internal regenerative program might pave the way for recovering lost brain functions.
Although there used to be doubt regarding the existence of adult neural stem cells, it is now well-accepted that neural stem cells exist in the adult brain. These stem cells play important roles in brain health and function, from supporting learning and memory to regulating mood in response to stressful conditions.
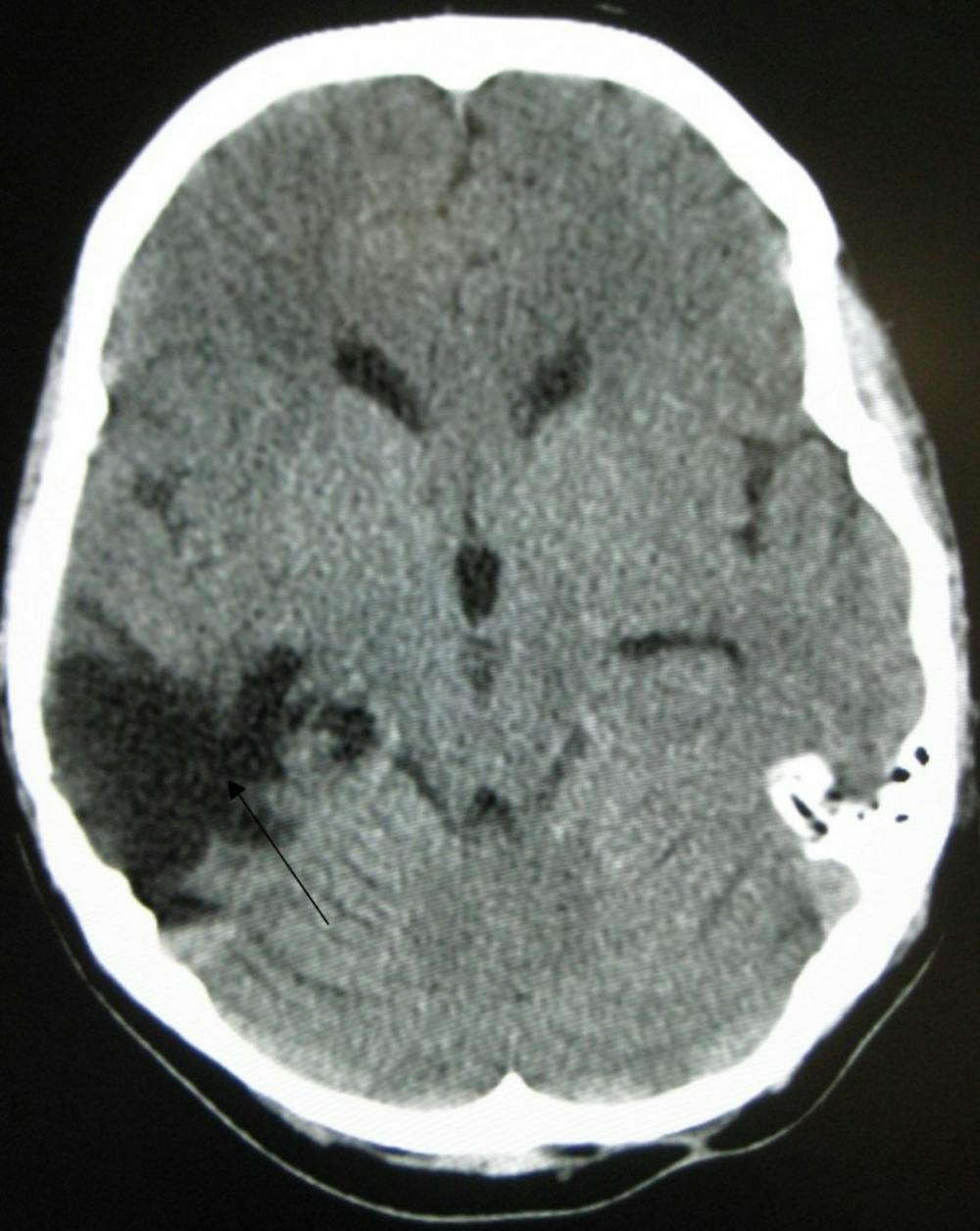
The existence of adult neural stem cells opens up major possibilities for endogenous brain repair. Indeed, some studies in rodent models showed that neural injury causes an increase in the proliferation of neural stem cells as well as the migration of stem cells toward the site of injury. Some of these observations have also been confirmed in human patients with traumatic brain injuries, suggesting that neural stem cells may have a reparative effect following injury.
In support of the hypothesis that increased neurogenesis plays a regenerative role in neural injury, reports have shown that preventing neurogenesis worsens cognitive decline following injuries. Altogether, these results suggest that it may be possible to enhance the human regenerative response to traumatic brain injuries by augmenting neurogenesis.
A big advantage of enhancing internal regenerative capacity via manipulating neurogenesis is that such a strategy can be accomplished non-invasively by possible medications. Other stem-cell-based strategies have focused on developing stem cell lines that are then surgically transplanted into human individuals. However, an obvious disadvantage of using externally developed stem cells is that an invasive surgery is required, and this may not be the optimal option for patients who are already physically fragile.
Despite the promise of this procedure, there are still major precautions that need to be taken when manipulating neurogenesis is considered as a therapeutic strategy. Although neural stem cells do migrate to areas of injury, evidence also suggests that they migrate and give rise to neurons at ectopic, or abnormal, locations. Such ectopic migration may actually be harmful since neurons at aberrant locations can lead to rewiring of neural circuitries that exacerbates the effects of traumatic injuries. Enhancing neurogenesis may inadvertently lead to the uncontrolled reorganization of neural circuits that further disrupt brain function.