Researchers at Rice University recently studied the effects of loneliness on the symptoms of the common cold. They found that patients who identified as lonely reported more acute cold symptoms while more sociable patients tended to report feeling less under the weather.
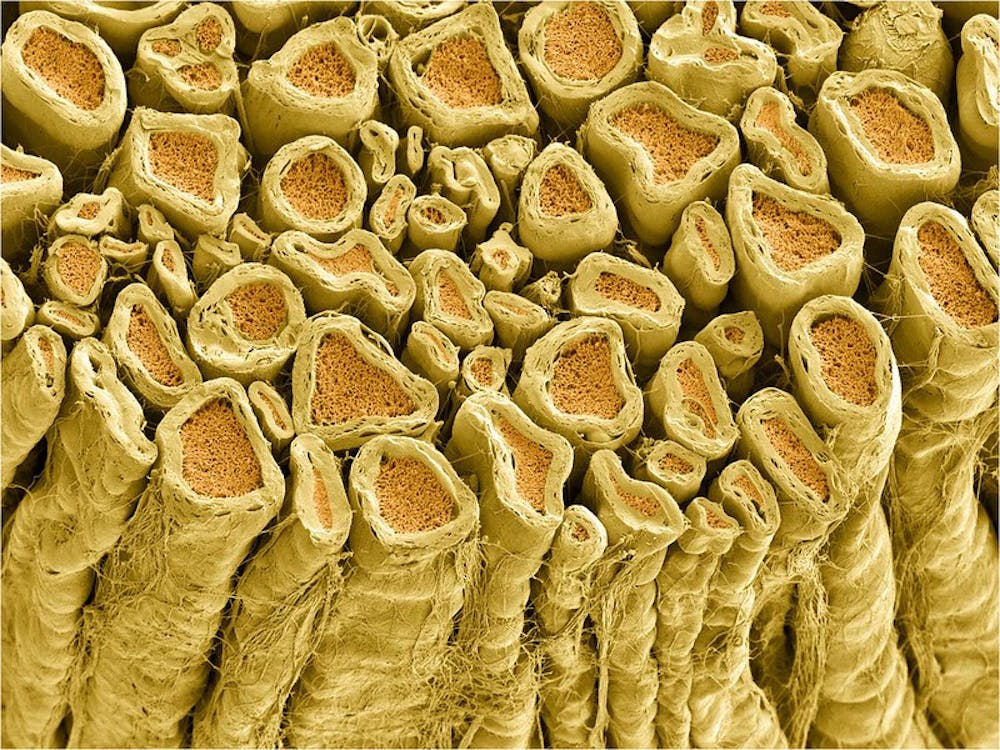
Common colds are caused by infection of rhinoviruses, one of the most prevalent infective viruses. Symptoms of a common cold typically include runny or stuffy nose, sore throat, cough and congestion. Patients can typically diagnose themselves and decide whether they wish to see a doctor or not.
“Previous research has shown that different psycho-social factors like feeling rejected or feeling left out or not having strong social bonds with other people do make people feel worse physically, mentally and emotionally,” Angie LeRoy, graduate student at Rice and one of the lead authors of the study, said in a press release. “So we had that general framework to work with.”
Specifically, previous studies have demonstrated that there’s a causation between loneliness and poor physical health. However, prior experiments proving that loneliness is risk factor for poor health have not looked at “patient reported outcomes” (PROs).
In clinical trials, researchers use PROs as questionnaires to help assess how well a therapeutic treatment works and to guarantee that patients will receive the best quality of care. PROs are also an important consideration for physicians when they treat their patients. Rather than treating each patient as a problem that needs to be solved, it may be more beneficial to understand the patients’ goals and the quality of life after treatment.
The researchers found that one of the contributing factors to common illnesses and diseases is an aspect of the patient’s quality of life — how lonely a patient is.
“Loneliness puts people at risk for premature mortality and all kinds of other physical illnesses,” LeRoy said. in the study “But nothing had been done to look at an acute but temporary illness that we’re all vulnerable to, like the common cold.”
The study, published in the journal Health Psychology, focused on differentiating between loneliness, social isolation and the two factors’ independent effects on the severity of the patient’s cold symptoms. It also studied whether loneliness or social isolation has a greater effect on the severity of a patient’s cold.
Two hundred thirteen patients completed the Short Loneliness Scale (LON), a 20-item metric designed to measure one’s subjective feelings of loneliness as well as feelings of social isolation.
Participants also filled out the Social Network Index, an assessment that takes into account both the quantity and quality of relationships.
“This paper is about the quality of your relationships, not the quantity,” LeRoy said in the study. “You can be in a crowded room and feel lonely. That perception is what seems to be important when it comes to these cold symptoms.”
The researchers then gave the study participants nasal drops so that they inhaled a rhinovirus, the infectious agent for common colds.
The team quarantined the infected patients for five days. During the quarantine, patients self-reported how they felt and how they thought they were doing while the team monitored heart rate, temperature and blood pressure.
“A predisposition, whether it’s physical or mental, can be exaggerated by a subsequent stressor,” Chris Fagundes, a Rice University psychologist, said. “In this case, the subsequent stressor is getting sick, but it could be the loss of a loved one, or getting breast cancer, which are subjects we also study.”
Fagrundes explained that this study’s specific focus makes it unique.
“It’s all about a particular predisposition (loneliness) interacting with a particular stressor,” he said.
Based on the results from 160 patients, the researchers concluded that if a patient gets sick when they’re feeling lonelier, they are at higher risk for more severe symptoms.
They found that it was not how many people patients counted among their close friends but rather how well they could count on those people and how close they felt to those people that indicated how lonely a patient felt.
Additionally, the researchers discerned that self-perception based loneliness, rather than standard and objectively measured social isolation, contributed greater to risk of feeling severely ill.
“We think this is important, particularly because of the economic burden associated with the common cold,” LeRoy said. “Millions of people miss work each year because of it. And that has to do with how they feel, not necessarily with how much they’re blowing their noses.”
The researchers suggest that being more socially active could have a positive impact on a patient’s physiological health. For those that have chronic illnesses and feel worse every time they fall ill compared to their peers, researchers recommend evaluating the social aspects of life.
“If you build those networks — consistently working on them and your relationships — when you do fall ill, it may not feel so bad,” LeRoy said.















Please note All comments are eligible for publication in The News-Letter.