
This illness, however, began to spread beyond Water Street. It was finally identified on Aug. 19 when Dr. Benjamin Rush, one of the most prominent American physicians of the time, announced that the cases were of yellow fever.
Philadelphia had not experienced a yellow fever epidemic in over 30 years, and the prospect of an impending one was terrifying.
Yellow fever symptoms were gruesome — high fevers, muscle aches, hemorrhage and the jaundice that gave the disease its name — and with no effective treatments, mortality rates could approach 50 percent.
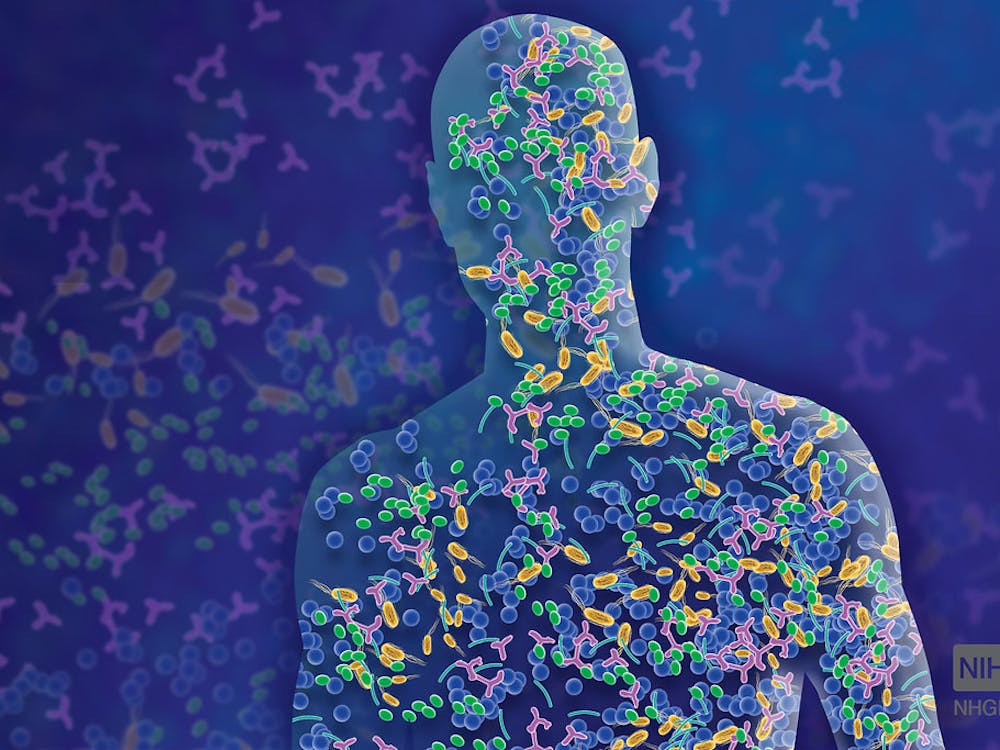
Furthermore, no one knew for sure what had caused it. There were two main competing theories. The first was that the disease was caused by a pestilential environment, and the second was that it was contagious and passed from person to person.
Personal opinions were influenced equally by everything from political leanings to religious beliefs to actual scientific reasoning.
As news of the disease outbreak spread, residents of Philadelphia began to flee the city by the thousands. Between late August and the end of the epidemic in mid-November of the same year, nearly 20,000 had left.
Those who remained were mostly poorer citizens who did not have the means to escape, along with some physicians and civil servants.
For those left behind, it was soon clear that recommended preventative measures were having little success in halting the epidemic. Residents fired guns inside their houses in hopes that it would clean the air and carried camphor and soaked handkerchiefs in vinegar.
Attempts were made to clean the streets, and there were calls to quarantine incoming ships, especially those bearing French refugees from the West Indies, who were thought by some to carry the disease.
Despite these efforts, the death toll proceeded steadily. By the end of August, an estimated 325 people had died, and in the next few months there would be almost 5,000 more victims, or 10 to 15 percent of Philadelphia’s pre-epidemic population.
For desperate Philadelphians, the pressing issue became how to treat yellow fever once it was contracted.
Here, just as with the cause of the disease, opinion split. The debate over treatment has often been visualized as one between progressive-minded physicians, mostly those of French origin, prescribing gentler treatments that we might accept today and stubborn traditionalists who were bleeding their patients into oblivion.
One of the more prominent advocates of milder therapy was Dr. Jean Deveze, a French doctor with experience practicing in the West Indies, who prescribed cinchona bark, wine, blistering of the skin, cold baths and bed rest.
In contrast, Rush and those who agreed with his methods believed firmly in the effectiveness of purging with emetics and laxatives, some of which contained mercury, accompanied by copious amounts of bloodletting.
While Deveze bled his patients too, Rush did so on an extreme level, sometimes recommending the removal of up to 80 percent of a patient’s blood.
At the time, however, it was not Rush’s methods that were considered traditionalist but Deveze’s. The French physician simply used what were the assumed treatments for yellow fever at the time, which Rush had in fact tried at first, only considering them ineffective after three of the four patients he treated in this way died.
Based in ancient principles of bodily humors, Rush’s procedures took older bleeding and purging treatments to unprecedented extremes.
Their drastic nature was partly influenced by a new concept Rush had developed himself: that there was only one disease in the world, which was associated with the blood vessels and could be resolved solely through depletion.
A nice end to this story would have been if the yellow fever outbreak exposed the dangers and fallacies of extreme treatment and led to less destructive (though hardly more curative) treatment.
Rush’s depletive regimen, sometimes labelled “heroic therapy,” weathered criticism, even as that criticism grew in intensity throughout the epidemic.
Later the methods were carried on by Rush’s pupils and applied to a variety of illnesses. There were numerous reasons why these treatments endured, including that they were novel, appeared to make sense from a certain contemporary conceptual standpoint and seemed better than doing nothing to combat disease.
The epidemic ended as soon as colder temperatures killed off the Aedes aegypti mosquitoes which we now know transmit yellow fever. Despite that, heroic therapy lived on.
It continued to hold sway over (and some even say dominate) American medicine for at least the next 20 years.



















Please note All comments are eligible for publication in The News-Letter.