
Known to the public only by his first name during his life (in order to protect the Vetters’ privacy), David captured the nation’s attention. He was periodically covered by the media, and his plight even made its way into pop culture.
But beyond this visibility, David’s situation also sparked an ethical debate, leading to a variety of advancements in health fields from immunology to oncology. These deeper issues ensured that the young boy’s impact would be more than being just a phenomenon.
David was moved into his first bubble less than a minute after he was born on Sept. 21, 1971 at Texas Children’s Hospital in Houston. Even before his birth, doctors and his parents knew that he would have a 50 percent chance of having SCID, and his older brother had suffered from the disorder.
The trait is commonly X-linked, suggesting that the boys’ mother was a carrier and thus any of her sons would have a coin-flip chance of inheriting the condition.
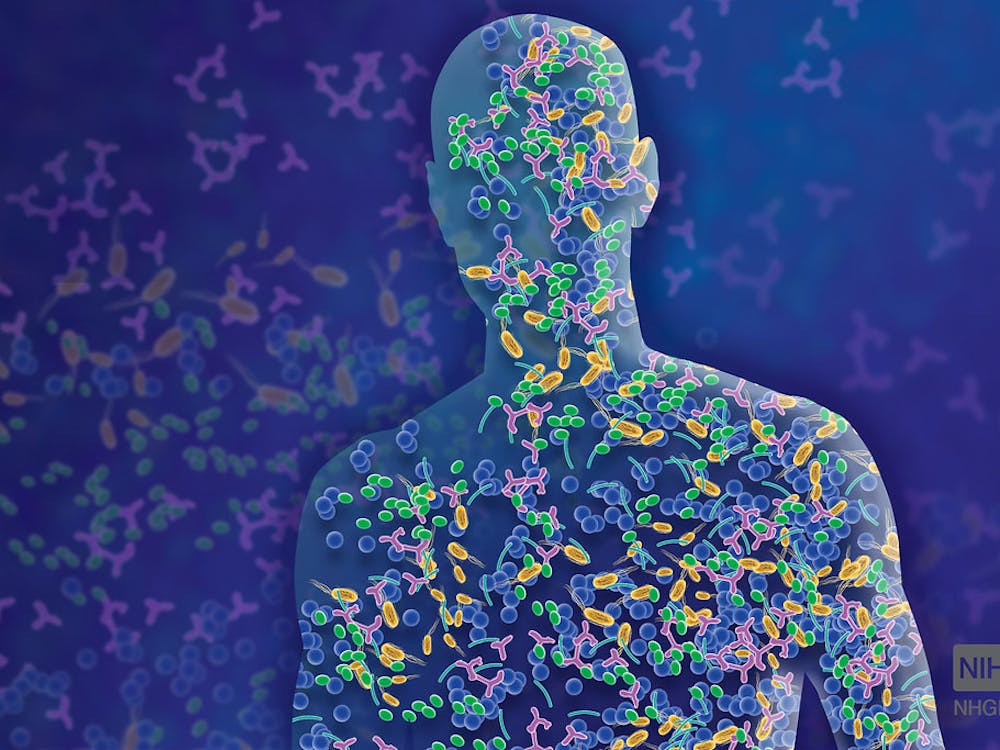
SCID involves a mutation on the X chromosome that causes deficient T lymphocytes, natural killer cells, as well as defective B lymphocytes. This results in a non-functioning immune system, and children with SCID usually die from infection within one to two years.
David’s own older brother had died at seven months, before he could receive a planned bone marrow transplant.
The Vetters’ younger son remained in isolation while they waited for the results of the blood test which would determine whether or not David had SCID.
The bubble was intended to be a temporary solution. However after it was discovered that David did in fact have the disorder and furthermore, that his sister Katherine was not a perfect match to donate bone marrow, it became the bubble became foreseeable reality while researchers hunted for a solution.
For the next twelve years, David grew up in a series of ever-larger plastic bubbles. There was one at his home, along with one at the hospital. David’s family held the young boy through thick gloves built into the sides of the chambers, and everything that entered the bubbles, from food to school supplies, was sterilized first.
When David was six, a “spacesuit” designed by NASA allowed him to venture outside at last. He only used it a few times.
The enclosures effectively kept David alive, but as he got older the ethical questions began to mount.
While media stories showed a seemingly optimistic, well-adjusted young boy, those who were with David daily, including nurses and the psychologist whom he had become close to, saw his anger and frustration and knew that he fully understood his situation.
Some questioned his quality of life and asked what would happen if the soon-to-be-teenager demanded to leave.
In the end, David would stay in the bubbles until he was twelve. During that time, advancements had been made in transplanting bone marrow that was not a perfect match. In 1983, David underwent a new procedure involving bone marrow from his sister, Katherine.
Though the transplant seemed at first to be a success, within a few months David became seriously ill and eventually left the bubble to be treated. He died on Feb. 22, 1984.
An autopsy revealed that Katherine’s bone marrow had contained the dormant Epstein-Barr virus, which, when introduced into the immunocompromised David, had caused lymphoma. The “bubble boy” had died of cancer.
It was this unpredicted development that was one of David’s greatest medical legacies. Dr. William Shearer, who had treated David, told the Los Angeles Times in 1985 of the significance. “It is the first conclusive evidence of cancer developing in a human being after infection by a virus,” he said.
Additionally, the extensive study conducted on David’s immune system significantly improved the understanding of both primary immunodeficiencies, such as SCID and secondary immunodeficiencies, including AIDS.
In the 1990s, his Epstein-Barr-infected immortalized B-cell line was also used to identify the genetic mutations that cause SCID.
In the present day, SCID can be treated using hematopoietic stem cell transplantation. Recently, gene therapy treatments are also being developed, which use retroviruses to insert a functioning copy of the mutated gene into a patient’s own stem cells.
Treatments are most effective when SCID is detected early, especially before infections set in. Beginning with Wisconsin in 2008, most U.S. states have implemented newborn screening for SCID, an important measure considering that children with SCID will appear healthy at birth.
Since David, there has not been another “bubble” child, and the hope is that, with modern screening and treatment procedures, there will never be another one.



















Please note All comments are eligible for publication in The News-Letter.