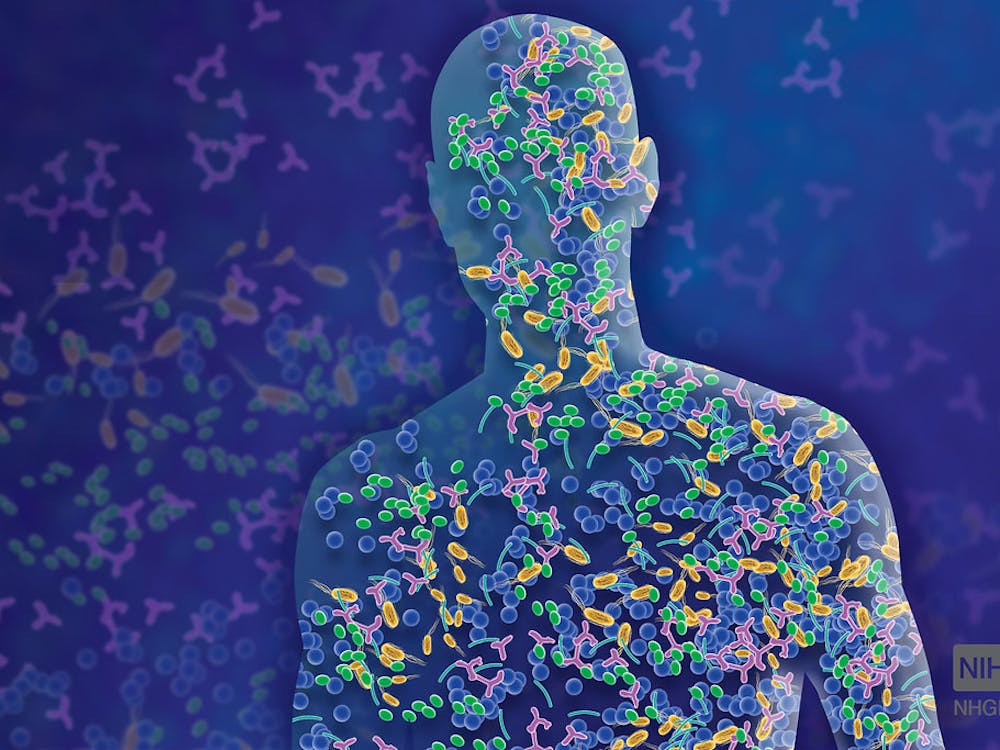
Temporary tattoos might someday become the primary form of treatment for chronic diseases such as multiple sclerosis. Nanoparticles called PEG-HCCs (polyethylene glycol combined with hydrophilic carbon clusters) were created in the lab of James Tour, a chemist at Rice University. They help inhibit T lymphocyte cells that sometimes mistakenly attack innocuous cells in the body.
These nanoparticles, which are selectively taken up by immune system cells, could help patients experience fewer side effects during treatment than during regular medication. By inhibiting only T cells and leaving other immune system cells like macrophages functional, PEG-HCCs help keep patients’ overall immune system intact.
In comparison, current immunosuppressant treatments are less selectively taken up by cells and act on a broader range. This inhibits other types of immune system cells, decreasing overall immune system strength and increasing the risk of getting infections.
Researchers at the Baylor College of Medicine discovered that these nanoparticles act as antioxidants and remove superoxide, an essential compound for T cell activation. By removing superoxide, PEG-HCCs limit the activation of T cells and inhibit their destructive effect on other cells in the body. In the case of multiple sclerosis, these PEG-HCCs may limit the destruction of myelin-producing oligodendrocytes by T cells and allow for better central nervous system functioning.
Patient treatment involves injecting the nanoparticles just under the surface of the skin. This, scientists assert, allows T cells to take up the particles more slowly and allows the medication to stay in one’s system longer than they would if the nanoparticles were directly injected into the bloodstream. The effects of the nanoparticles last approximately one week, and researchers consider a week the optimal duration for treatment. A week gives the compound enough time to take effect but is short enough that doctors can easily curtail the treatment if a patient reports adverse effects.
During the week after injection, a dark spot will appear at the injection site. These marks, which fade after a week, can be shaped into tattoo designs by micropattern needles or placed in hidden areas.

In lab studies on rodents, these nanoparticles showed no sign of acute toxicity, so this treatment could soon become more widespread. Researchers hope that the similar nanoparticles could soon be used to deliver cancer drugs to tumors and treat other autoimmune diseases.
On the Hopkins campus, nanoparticles have already been used to eliminate cancerous brain cells. Associate Professor of Biomedical Engineering (BME) Jordan Green and other researchers at Hopkins have successfully used biodegradable nanoparticles to kill glioma cells in rats. In a study on the American Chemical Society’s Nano website, Hopkins researchers used ganciclovir and nanoparticles loaded with the enzyme herpes simplex virus type 1 thymidine kinase (HSVtk), to kill lab-grown glioma cells with 100 percent efficacy.
Although the process still involves injection directly to the brain, researchers hope that the treatment can be administered more systematically in the future.
Perhaps in the future, nanoparticle treatments will replace injections and invasive treatments as more permanent remedies for chronic diseases.




















Please note All comments are eligible for publication in The News-Letter.