By MANISH PARANJPE Senior Staff Writer
According to the Harvard T.H. Chan School of Public Health, the United States is facing an obesity epidemic. Americans are getting heavier every year, which increases their risk of developing cardiovascular disease, hypertension, diabetes, stroke and sleep-disorders. But a high fat diet may do more than cause these metabolic problems. According to this new study, obesity could be linked to changes in brain chemistry.
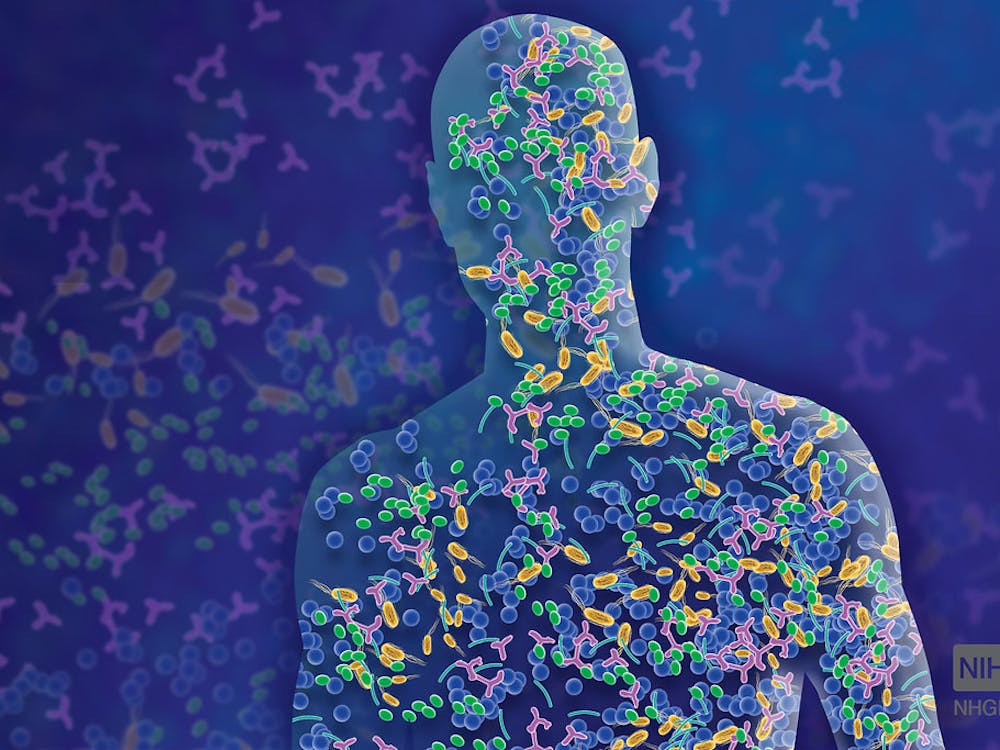
In a study published in the journal Brain, Behavioral, and Immunity, researchers found, for the first time, that a high fat diet can cause the immune cells of our nervous system, microglia, to become active and start eating away at our neuronal connections. But there is still hope for the burger-lovers among us: The researchers also found that after switching to a low fat diet, these neuronal problems could be corrected.
For their study, Dr. Alexis Stranahan, along with his colleagues at the Medical College of Georgia, fed mice either a high fat diet (HFD) or low fat diet (LFD) for three months. After three months, some of the mice with the HFD were switched to a LFD for two more months, while the rest were kept on a HFD. The mice initially fed a LFD were maintained on this diet for the full five months. Throughout the course of the experiment, the researchers monitored measures of the mice’s metabolism including weight, average calorie intake, fat pad weight, blood insulin and glucose levels. In addition to these measures of obesity, Stranahan and his team also measured several indicators for microglia activation and synaptic function.
Microglia, immune cells of our nervous system that promote inflammation in the brain, are critical in maintaining properly functioning neurons.
“Normally in the brain, microglia are constantly moving around. They are always moving around their little fingers and processes. What happens in obesity is they stop moving,” Stranahan told Science Daily. “They draw in all their processes; They basically just sit there and start eating synapses. When microglia start eating synapses, the mice don’t learn as effectively.”
After 12 weeks, the mice that were initially fed a high-fat chow experienced weight gain and an increased weight of adipose tissue, or fat tissue, in their pads. Switching back to a low fat chow after 12 weeks reversed this weight increase, but only partially.
After confirming the presence of obesity, the team moved to analyze synaptic and microglial activity in the hippocampus, the center of learning and memory. Stranahan found an increased level of cytokines, small inflammatory molecules produced by hippocampal microglial cells upon activation, in the mice fed the HFD. They also found that microglia in the obese mice ate more synapses than those in the low-fat diet mice.
In addition to microglia, hippocampal synapses in high-fat-eating mice changed. After monitoring the electrical properties of the mice’s hippocampi using electrophysiology, the researchers found that hippocampal synapses in the high-fat-eating mice became less sensitive.
In memory-dependent tasks, the obese mice had significantly lower spatial memory and object recognition abilities, signs of a weakened hippocampus.
After 12 weeks, the researchers switched the obese mice to a low-fat chow. After the switch, Stranahan found that microglial and hippocampal synaptic activity returned to their baseline levels. Diet reversal, as the authors explained, seems to normalize obesity-related changes in the brain.
The team also found that, even after 12 weeks of being on a high fat diet, the mice had no insulin resistance, indicating that changes in the brain take place before the onset of diabetes.
Microglia are critical for maintaining healthy synapses. During normal physiological conditions, microglia serve to prune synapses that are not working properly, ensuring healthy brain development. However, as Stranahan’s research suggests, obesity alters this careful balance. The good news is that the brain changes that happen as a result of obesity are largely reversible with proper dieting.
The study notes that, while mice were on the HFD, they still ate same the amount of calories as mice on the LFD.
“The entire metabolic phenotype is driven by diet composition rather than the amount of calories,” Stranahan told Science Daily.
Thus, if high-fat-eating mice had greater variety in their diets, they might also have consumed more total calories, as humans often do.



















Please note All comments are eligible for publication in The News-Letter.