Antibiotics are the most commonly prescribed medicine in the United States, but are they always really necessary?
According to the Centers for Disease Control and Prevention (CDC), doctors prescribe up to 18 million courses of antibiotics a year for the common cold despite the fact that colds are typically caused by viruses. This overuse of antibiotics, combined with people not following instructions when taking them, has led to the evolution of antibiotic-resistant bacteria. A recent Hopkins study focused on some of the reasons that doctors might overprescribe antibiotics.
During ancient times, the Greeks and Indians used molds and plants to treat infections. In fact, in Greece and Serbia moldy bread was traditionally used to treat wounds. In 1928, Sir Alexander Fleming discovered the antibiotic property of penicillin from the fungus Penicillium notatum for which he was knighted and was given the Nobel Prize in Physiology or Medicine in 1945.
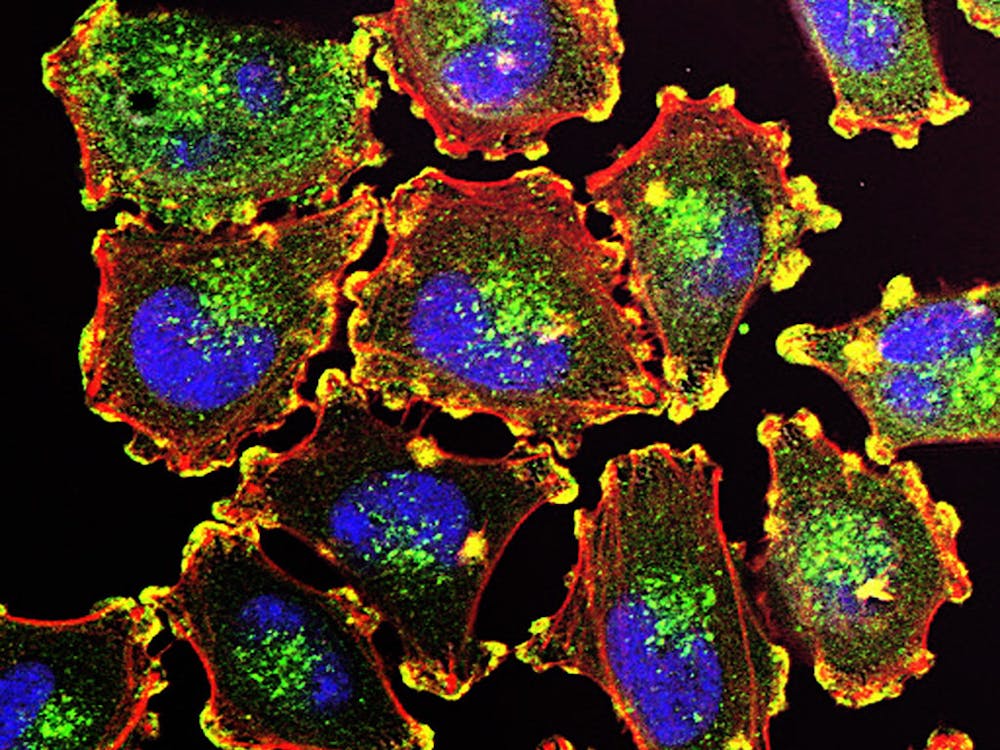
Bacteria cause most infections in our bodies. If our immune system is compromised or overwhelmed, we can be treated with an antibacterial group of chemical compounds known as antibiotics to treat the infection. Antibiotics are meant to be used to treat only bacterial infections and are not effective against viral infections such as most sore throats and the flu.
Antibiotics, however, have been used so widely and for so long that the infectious organisms the antibiotics are designed to kill have adapted to them, making the drugs less effective, or in increasingly numerous cases, completely ineffective. Each year in the United States, at least two million people become infected with bacteria that are resistant to antibiotics, and at least 23,000 people die each year as a direct result of these infections.
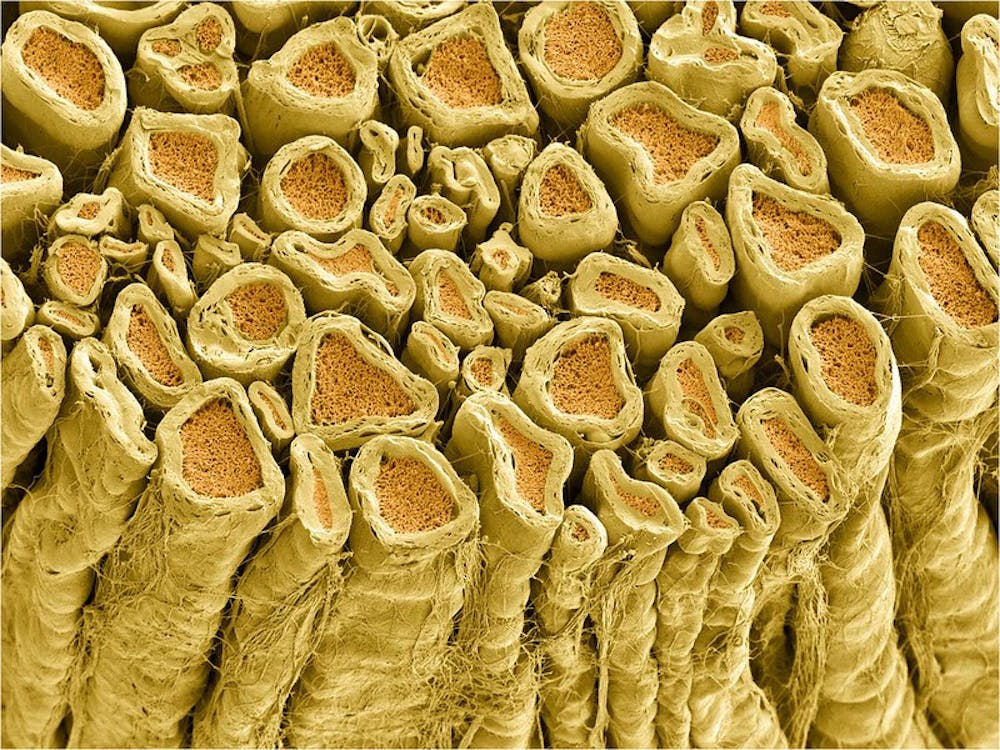
Bactericidal antibiotics work in one of two ways: killing the bacteria by interfering with the bacterium’s cell wall and contents, or preventing bacteria from successfully multiplying by interfering with protein production, DNA replication or some aspect of their metabolism.
Recently, a group of researchers led by Hopkins scientists have found that competition among medical establishments in wealthy areas of the U.S. leads to an increase in the number of antibiotic prescriptions written.
The researchers reported in the Journal of Antimicrobial Chemotherapy that they found that the number of physicians and clinics per capita affect the number of antibiotic prescriptions written.
The highest rates were found in the southeastern U.S. and along the East and West Coasts. Manhattan is the area that prescribes the most antibiotics, followed by southern Miami. Overall, the prescription rate varied widely across the U.S.
Data for this study was obtained from the U.S. Census Bureau and the IMS Health Xponent database, which tracks prescriptions dispensed at the ZIP code level. According to the findings, an increase in prescribing rate exists where retail medical clinics are located, which are similar to those found in chain drug stores and super stores. However, the effect was different in wealthy versus poor regions.
According to the research team, the findings add to the evidence indicating that economic and social factors are contributing to the increasing problem of overuse of antibiotics in the U.S. The CDC recently released a statement reporting that this type of overuse is a major contributing factor in the spread of antibiotic resistance and is a worldwide public health threat.
Also, the results of the study suggest to the researchers that in wealthy areas patients may shop around for a physician who is more likely to write a prescription for antibiotics than would happen with patients in poorer areas. One of the researchers, Eili Klein of the Hopkins School of Medicine, commented that they felt the study suggested that in certain areas, doctors are in competition with other doctors. This competition makes physicians feel pressured to prescribe antibiotics.
The study authors are hopeful that their results will contribute to a better understanding of the reasons for antibiotic overuse and that the findings will also be used to develop measures to reduce inappropriate antibiotic-prescribing behavior.



















Please note All comments are eligible for publication in The News-Letter.