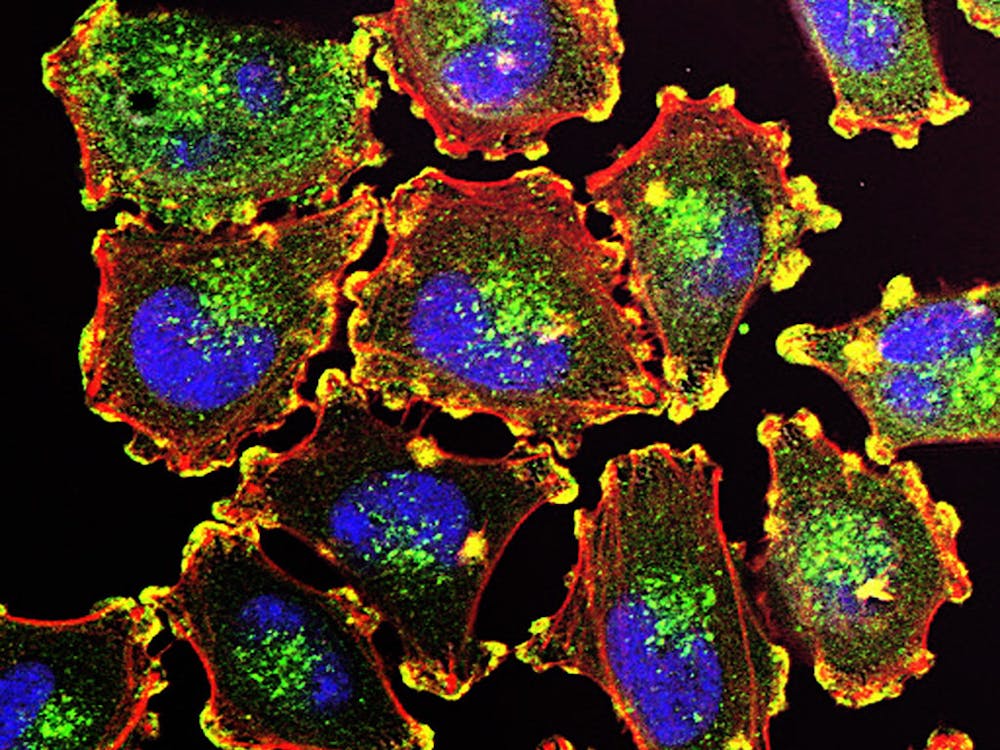
From the perspective of medication, human immunodeficiency virus (HIV) is the most dangerous when it’s asleep. While active subsets of the virus can be destroyed with antiretroviral agents, dormant viral particles can accumulate within the T cells of the immune system without detection. These dormant particles significantly compromise the T cells’ abilities to recognize and destroy infectious cells in the body. With dormant strains of HIV, the T cell is about as effective as shampooing your hair with dirt.
Hopkins scientists have been researching strategies to activate the residual viruses in T cells. By inducing the virus into an active state, it can be targeted by the same drugs that treat active HIV. This would hit a larger portion of the cells infected with HIV and thereby reduce the virus’s ability to reproduce.
Unfortunately, none of the promising strategies have worked so far. One complicating factor is the need for rigorous adherence to medication after the virus is activated. If an individual stops taking medication after the active portions of the virus have been cleared, the dormant portions of the virus can reactivate, reproduce and eventually repopulate the body.
Another complicating factor is the inability of conventional blood tests to determine latent viral loads. This makes it difficult for researchers to determine the proper HIV activation protocols. In fact, this viral hibernation effect is one of the reasons HIV is so insidious. When cornered and threatened with elimination, the virus slows down production of proteins.
Compounds called HDAC inhibitors were tested to awaken the infections and make them vulnerable to eradication. Essentially, these inhibitors prompt the translation of infectious DNA sequences. If used in conjunction with RNA-specific medication, the newly active sequences can be targeted for destruction. HDAC inhibitors have been used successfully in treating some cancers and neurological disorders by disrupting viruses at the RNA level.
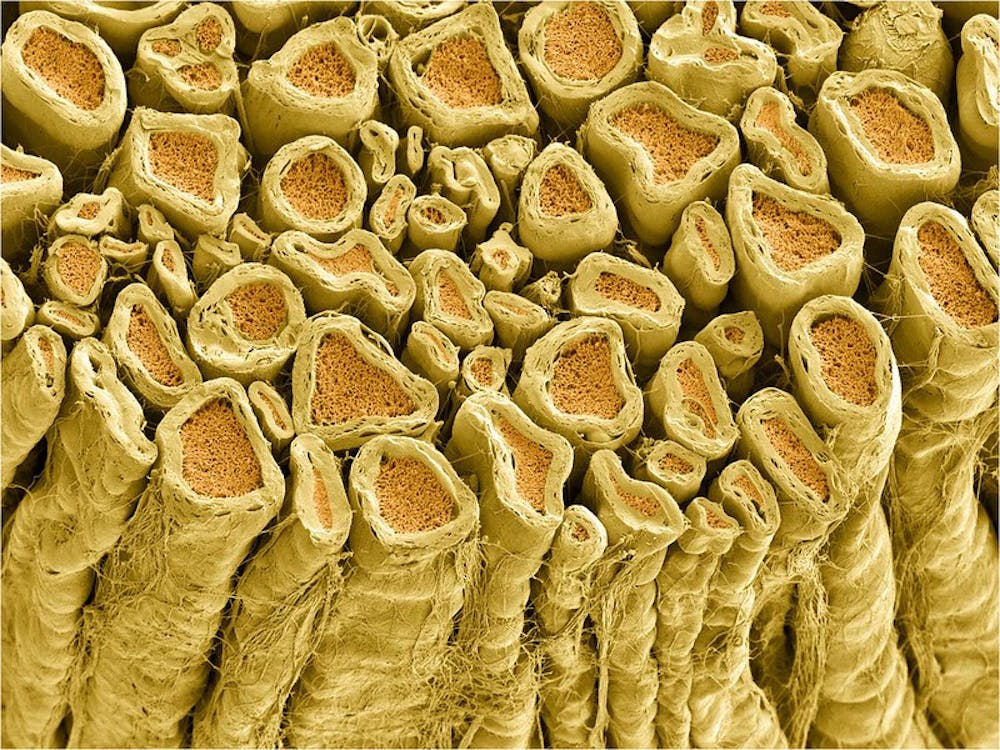
After separating red and white blood cells from infected patients, the HDAC method was tested for HIV-infected patients. The treatment wasn’t successful for targeting infected white blood cells, and this inadequacy came as a surprise to researchers.
Scientists are now investigating methods to create more sensitive assays to find and locate viruses in hopes of increasing the efficacy of targeting agents. Although these recent results are disheartening, HIV research is still advancing forward.



















Please note All comments are eligible for publication in The News-Letter.