Researchers have named a now two-and-a-half year old child the first infant “functionally cured” of HIV following rapid antiretroviral treatment after birth. Deborah Persaud, lead author of the report and a virologist at the Hopkins Children’s Center, made the announcement along with her two co-investigators in Atlanta on Sunday at the 20th Conference of Retroviruses and Opportunistic Infections.
“This is a great case, generating many important questions as well as hope for many babies born to HIV-infected mothers,” Kwang Sik Kim, chief of Pediatric Infectious Diseases at the Hopkins Children’s Center, wrote in a statement.
The “functional cure” achievement means that without treatment, the child has remained in long-term remission with no viral replication detectable through typical clinical tests. The researchers say that a normal lifespan is expected and that the patient is unlikely to be able to transmit the virus to anyone else.
The infant, whose identity is being protected, was treated at the University of Mississippi Medical Center by Hannah Gay, who acted quickly after realizing just how high at risk this newborn was for HIV infection.
The child’s mother received her HIV-positive diagnosis while in labor.
Normal medication could not be administered at that point. This, compounded with the complete lack of very effective prenatal antiviral therapy, left the child at great risk. (The researchers later confirmed that the child’s infection occurred momentarily before birth.)
Gay decided to take a more aggressive approach to post-delivery care than the typical prophylactic treatment of at-risk infants. She administered antiretrovirals, the common therapy for HIV, within only 30 hours of the child’s birth, and added two medicines to the typical drug regimen. Gay was under the assumption that the patient would continue treatment for a lifetime.
What happened next was unexpected.
Over the ensuing month, the child’s viral load — a measurement of the amount of virus in the blood — decreased so significantly that it was undetectable by standard clinical tests. Despite the fact that the mother failed to bring the infant to scheduled appointments or to continue treatment from the ages of 18 to 23 months, the child’s load measured consistently under detectable levels at the first appointment back.
This result surprised Gay and specialists Persaud and Katherine Luzuriaga, an immunologist at the University of Massachusetts Medical School, who were called in for suggestions and further investigation. Again, tests found no evidence of viral replication.
“To our knowledge this is the first case of thoroughly documented perinatal HIV transmission that later remained undetectable for the long-term off of medications,” Gay wrote in a statement.
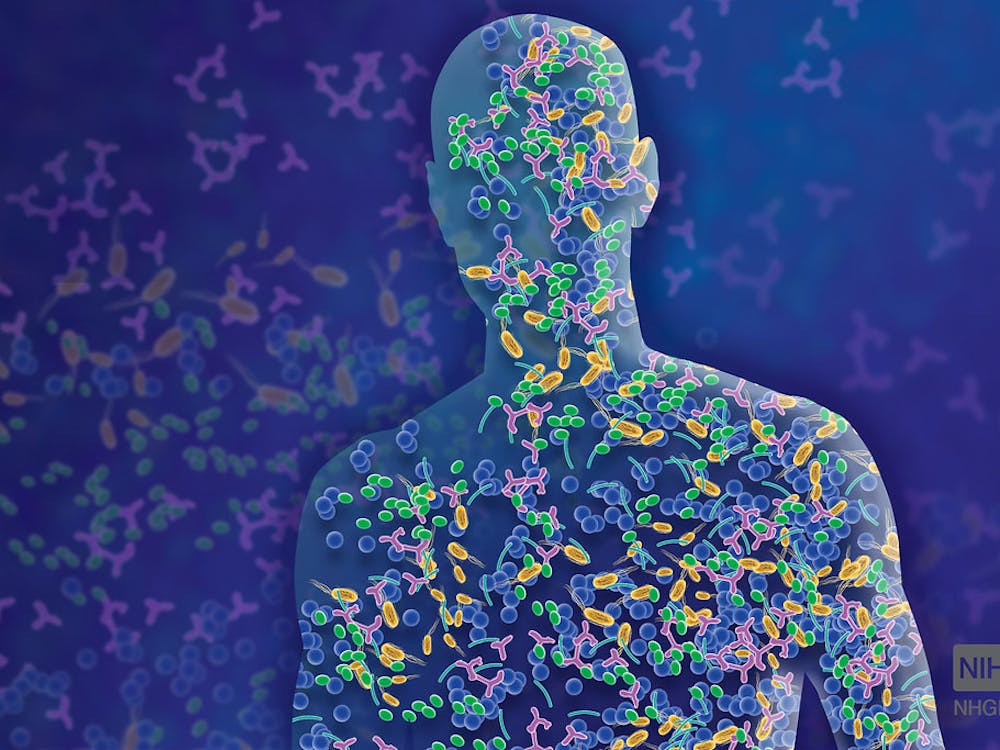
“Our hypothesis that needs careful testing is that the very early administration of potent combination therapy may have prevented the entry of the virus into the long-lived cells of the immune system where it stays for many years.”
Gay refers to the viral reservoirs where HIV typically spreads and effectively hides from all treatment. Even when antiretrovirals kill the virus’ replication mechanism in a patient’s short-lived immune cells, the virus hidden in these caches will reemerge if treatment is discontinued.
With approximately 9,500 people living with perinatally-acquired HIV at the end of 2009, according to the Centers for Disease Control and Prevention (CDC), the researchers are left with the pertinent questions of what caused the “functional cure” and whether it can be replicated in other infected infants.
“The early treatment most likely contributed to the outcome in this child. But whether it’s the only intervention that allowed this outcome is unclear and requires further study,” Persaud said in a question and answer session on Monday.
As research continues, the doctors urge HIV-infected infants to continue antiretroviral therapy without going off treatment to see if similar results occur. They also continue to advocate for antiviral treatment for expectant HIV-infected mothers, which, according to the CDC, can prevent over 99 percent of the risk of mother-to-child transmission.



















Please note All comments are eligible for publication in The News-Letter.